Abstract
Erythroid terminal differentiation (ETD) entails cell divisions coupled to decreasing cell size. The tight link between the number of cell divisions and red cell size is apparent in nutritional deficiencies or genetic variants in which fewer cycles result in larger red cells. Here we investigated novel EpoR functions, finding that EpoR signaling disrupts the relationship between cell cycle number and cell size, simultaneously promoting rapid cycling and the formation of larger red cells.
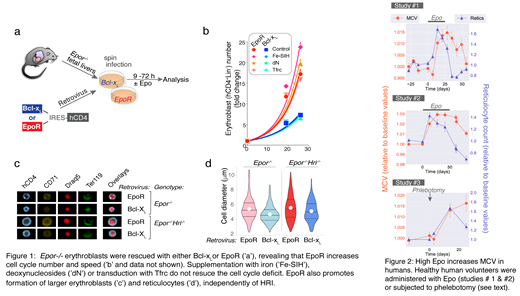
EpoR is essential for erythroblast survival, but it is unclear whether it has other non-redundant functions. To address this, we developed a genetic system in which we rescue mouse Epor -/- fetal liver progenitors from apoptosis by transduction with the anti-apoptotic protein Bcl-x L, and compare their ensuing differentiation with that of Epor -/- progenitors rescued with EpoR (Fig 1a). We found that the Bcl-x L survival signal, in the absence EpoR, supported formation of enucleated red cells. However, key ETD features were abnormal.
First, Bcl-x L-transduced Epor -/- erythroblasts underwent slower and fewer cell cycles (Figure 1b), differentiating prematurely into enucleated red cells. Premature induction of the cyclin-dependent-kinase inhibitor p27 KIP1 was in part responsible for the fewer cycles in the absence of EpoR signaling. We confirmed that EpoR also stimulates rapid cycling in wild-type erythroblasts in vivo, using a mouse transgenic for a live-cell reporter of cell cycle speed.
Second, using imaging flow cytometry, we found that Bcl-x L-transduced Epor -/- erythroblasts were smaller than EpoR-transduced Epor -/- cells (Fig 1c,d). By doubly transducing Epor -/- erythroblasts with both Bcl-x L and EpoR, we verified that EpoR absence, and not Bcl-x L overexpression, is responsible for the smaller size of Bcl-x L-transduced Epor -/- erythroblasts and reticulocytes.
Bcl-x L-transduced Epor -/- erythroblasts failed to upregulate the transferrin receptor, suggesting that iron deficiency may be responsible for their smaller size. However, neither iron supplementation, nor transduction with the transferrin receptor, rescued their smaller size. Iron regulates cell size through Heme-regulated eIF2α kinase (HRI). To definitively test the role of iron and HRI, we generated mice doubly deleted for both EpoR and HRI. We then rescued both Epor -/- and Epor -/-Hri -/- -fetal liver cells in parallel, by transduction with either Bcl-x L or EpoR. In agreement with the known role of HRI as a negative regulator of erythroblast size, both Bcl-x L- transduced and EpoR-transduced erythroblasts were larger on the Epor -/-Hri -/- genetic background. However, the difference in size between Bcl-x L and EpoR-rescued erythroblasts persisted in Epor -/-Hri -/- erythroblasts and reticulocytes (Fig 1c,d), conclusively showing that EpoR signaling regulates cell size independently of the HRI pathway.
EpoR promoted increased erythroblast and reticulocyte cell size in wild-type mice in vitro and in vivo, in response to Epo concentrations ranging from 10 to 10,000 mU/ml. We also evaluated the effect of Epo on red cell size in humans, in two independent studies, where healthy volunteers were administered Epo for either 3 weeks (20 IU /kg every 48 hours, 25 subjects, Study #1) or for 7 weeks (weekly Epo dosing that increased hemoglobin by 10 -15%; 24 subjects, Study #2). In a third intervention, 21 subjects participated in a randomized double-blind placebo-controlled crossover study in which 900 ml of whole blood was withdrawn from the treatment group by venipuncture. In all three studies, the increase in MCV in the treatment groups persisted long after Epo and reticulocyte levels returned to baseline (Figure 2). There was no correlation between MCV and the reticulocyte count, whose time courses were clearly divergent (r < 0.1, Pearson's product-moment correlation). Further, computational simulation suggests that the extent and duration of the increase in MCV is unlikely to be the result of skewing of the circulating red cell population in favor of younger, larger red cells.
Our work reveals a paradoxical EpoR-driven increase in erythroblast cycling simultaneously with increased erythroblast and red cell size. It suggests that EpoR alters the relationship between cell cycle and biomass in erythroblasts. It further suggests that hypoxia, anemia and other high-Epo syndromes are new diagnostic interpretations of increased MCV in the clinic.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal